 Supporting patients can be complex. Their acute or chronic illnesses may need care coordination across services.
Supporting patients can be complex. Their acute or chronic illnesses may need care coordination across services.
In comes the case manager.
Patient case managers connect patients to services and resources to better understand and manage their illness, avoiding unnecessary hospitalizations for improved, cost-effective health outcomes.
Case managers can find and communicate with endocrinologists and ophthalmologists for patients living with diabetes. They work with renal specialists and mental health services on behalf of members suffering lupus. They direct members to disease management programs for education tools, and identify the social and physical determinants derailing patient therapy adherence. Hastening patient speed to therapy, case managers find financial programs for patients who need assistance paying for medication and address reimbursement issues.
Coordinating fragmented services for high-risk members, who may be dealing with multiple complex conditions, can be a lot to manage. So how can case managers effectively support 150 patients, ensuring no one slips through the cracks? Who supports case managers while they support patients?
Why case management software?
To best oversee the patient journeys of a large pool of members, case managers need to rely on good software. Innovative software reduces ambiguity and time waste by creating a rules engine to guide managers through their patient workflow. Configuring software to prompt patient communication, which records all data and interactions for consistent messaging between care teams, case managers know their patients are receiving the steady support they need.
In value-based healthcare, it is necessary to anticipate problems before they happen and take preventative approaches towards case management. In order to do this, case managers must respond to the underlying data in front of them to see the potential problems before they occur.
Traditional case management software is not designed with proactivity (or healthcare) in mind. It equates people to tickets. It doesn’t recognize opportunities for patient intervention, nor alert case managers when specific people need attention. The dashboards reflect some “ticket” data, rather than the scope of the person’s care. The instinct for this software is designed to close tickets over a short period of time rather than proactively manage patients over an extended period. Welkin is different.
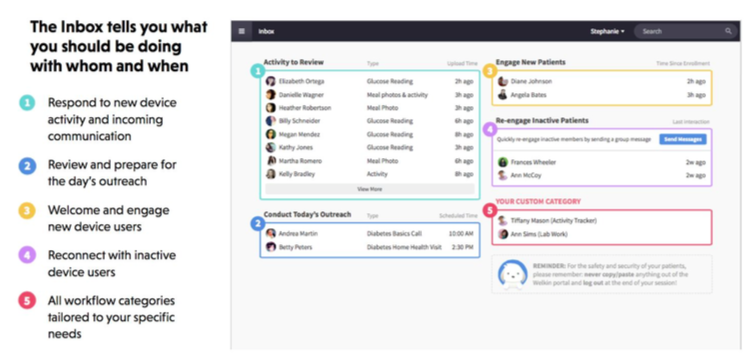
Welkin’s solution Welkin first centralizes all patient data into one place and then puts rules on top of it that govern the when, why, and how of a case managers work with patients. Situations like “if we receive a denial request, then do X, Y, and Z” or “if this patient has an ER visit, then do the following” are the lifeblood of Welkin’s inbox. It is this inbox / rules engine that allows us to encode proactive healthcare into a format that’s doable for case managers. It’s not uncommon to hear quotes from case managers on our platform like:
Welkin first centralizes all patient data into one place and then puts rules on top of it that govern the when, why, and how of a case managers work with patients. Situations like “if we receive a denial request, then do X, Y, and Z” or “if this patient has an ER visit, then do the following” are the lifeblood of Welkin’s inbox. It is this inbox / rules engine that allows us to encode proactive healthcare into a format that’s doable for case managers. It’s not uncommon to hear quotes from case managers on our platform like:
“Lots of times when I contact a patient from Welkin they say they appreciate us being proactive in our communications and they like being able to reach us when needed.”
“Helps me everyday to provide better service to each patient I speak with by tracking my calls and letting me know when it is time to check in again.”
“Looking back at previous data has allowed us to focus on when they got relief and circle back to optimize that area.”
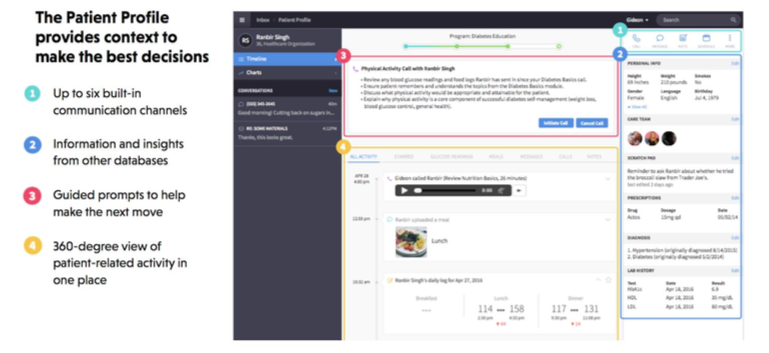
After creating the rules that govern a case managers interactions with patients, Welkin is able to centralize all communication and workflow into a single place, often consolidating multiple pieces of cobbled-together tools into one extremely useful piece of software. This patient profile, for example, is the only view that other case management software typically provide, and alone is insufficient to handle the complexities of healthcare.
Unlike traditional case management software, Welkin does not focus on configurability at the user interface level, and instead focuses on configurability at the workflow level. This matters. Given our already best-practice UI, we can cut down on configuration costs dramatically and increase speed to deployment for our customers.
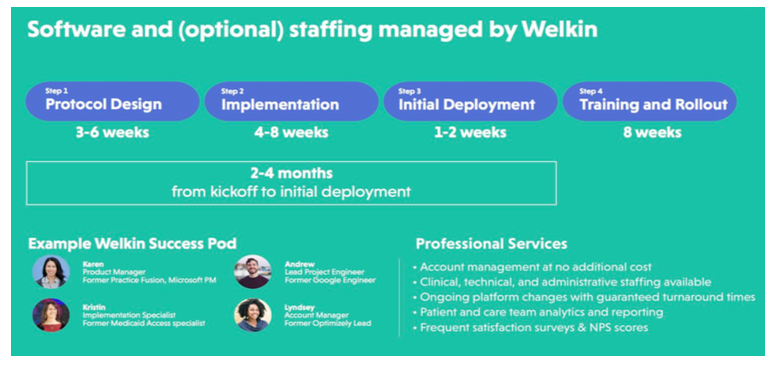 Moreover, the intense level of configuration on workflow and business process allows us to tailor our software to a variety of situations. This is paramount for healthcare organizations using a complex process to ensure that no patient falls through the cracks. The benefits of using software actually designed for healthcare is that their needs have already been considered, like compliance support, and implementation specialists who are experts in domain-specific workflow design.
Moreover, the intense level of configuration on workflow and business process allows us to tailor our software to a variety of situations. This is paramount for healthcare organizations using a complex process to ensure that no patient falls through the cracks. The benefits of using software actually designed for healthcare is that their needs have already been considered, like compliance support, and implementation specialists who are experts in domain-specific workflow design.
Welkin understands the complexity of patient management, and the need for a software solution that meets these intricacies so that case managers can focus on what matters most- patient care.



 This week, World Congress’
This week, World Congress’ 
 Managing one’s own chronic disease can be tricky. Coordinating therapies with everyday life takes a lot of practice, as does
Managing one’s own chronic disease can be tricky. Coordinating therapies with everyday life takes a lot of practice, as does 

 When Apple announced how the Apple Watch’s new bluetooth API can integrate directly with the Dexcom sensor,
When Apple announced how the Apple Watch’s new bluetooth API can integrate directly with the Dexcom sensor,